Why Yeast Infections Are More Common After Hysterectomy — And How to Prevent Them Naturally
By Dr. Shawn Bladel | July 13, 2025 | Recreated Health
For many women, a hysterectomy brings relief from years of pain, heavy bleeding, or other health struggles. But one common side effect that isn’t often talked about is the increase in yeast infections afterward. If you’ve noticed this pattern, you’re not alone — and there are clear biological reasons why it happens, along with practical steps you can take to reduce your risk.
Why Yeast Infections Increase After Hysterectomy
1. Hormonal Shifts
Even if the ovaries are left intact, blood flow to them can decline after hysterectomy. This often reduces estrogen production earlier than expected. Estrogen is critical for vaginal health — it thickens the tissues, helps maintain lubrication, and supports healthy levels of protective bacteria (Lactobacillus). Lower estrogen leads to a higher vaginal pH, which creates the perfect environment for Candida (yeast) to grow [1,2].
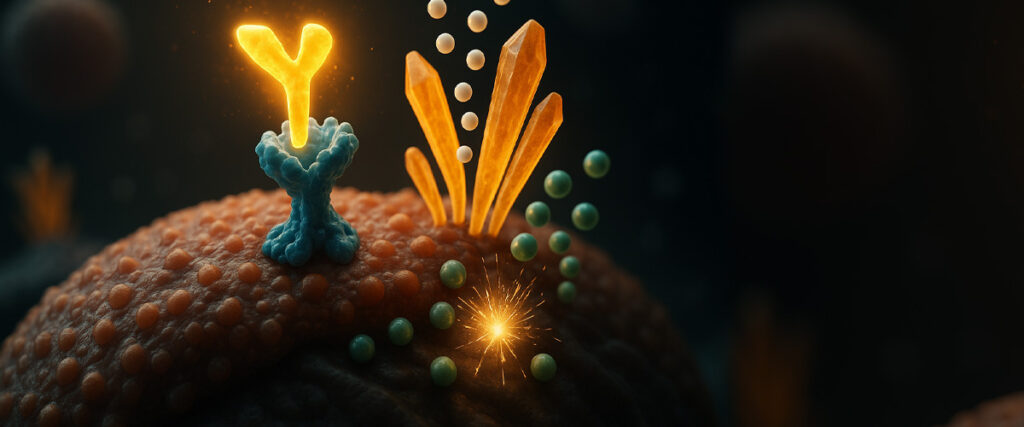
2. Loss of Local Immune Barriers
The cervix doesn’t just connect the uterus and vagina — it also plays a role in local immunity. Cervical mucus and immune proteins help protect against infections. When the cervix is removed, some of this protective barrier is lost, lowering natural defenses [3].
3. Antibiotic Use During Surgery
Most women receive antibiotics during and after hysterectomy to prevent surgical infection. While important for surgical safety, antibiotics also wipe out healthy gut and vaginal bacteria, giving yeast an opportunity to overgrow [4].
4. Stress & Recovery Burden
Surgery itself is a major stressor. Healing requires energy, and oxidative stress rises during recovery. This can suppress immune function and mitochondrial energy production, both of which normally help keep yeast in check [5].
How to Reduce Yeast Infection Risk Naturally
Support Estrogen Balance
- Add phytoestrogen-rich foods like ground flaxseed and legumes.
- Consider a high-quality hormone-balancing supplement (e.g., FemGuard + Balance by Designs for Health).
- Discuss bioidentical hormone therapy with a practitioner if needed.
- If you would like to get a complete picture of your estrogen hormones and pathways, along with an adrenal/cortisol picture, click this link to read about the DUTCH test, which is an easy-to-complete, at-home urine test for comprehensive hormones.
Restore the Microbiome
- Use probiotics with clinically studied strains for vaginal health, such as Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 (found in Fem-Dophilus® Jarrow Formulas).
- For gut and immune support, ProbioMed 100 (Designs for Health) is an excellent option.
- Vaginal probiotic suppositories (FloraFemme or VagiBiom) can help repopulate good bacteria directly.
Maintain Vaginal pH
- Consider boric acid suppositories (pH-D Feminine Health).
- Use only unscented, gentle cleansers externally (such as Dr. Bronner’s Baby Unscented).
- Avoid chemical douches, which disrupt the microbiome.
Strengthen Immune & Mitochondrial Health
- Optimize vitamin D (blood levels 70+ ng/mL; consider Vitamin D Supreme).
- Support mitochondrial resilience with MitoActive (CellCore) and magnesium glycinate.
- Eat nutrient-dense, anti-inflammatory foods and reduce processed sugar.
Choose the Right Underwear
- 100% organic cotton is best for breathability.
- Bamboo or hemp blends are good alternatives.
- Avoid synthetic fabrics, thongs, and overly tight underwear, which trap heat and moisture.
Why the Liver, Gut, and Thyroid Matter
- Liver Health: The liver clears excess estrogen and toxins. A sluggish liver makes hormonal balance harder to maintain and may increase candida risk [6]. Supporting detox pathways with KL Support (CellCore) or a Liver Glandular can help.
- Gut Health: 70% of immune function lives in the gut. Dysbiosis fuels candida, and gut bacteria also recycle estrogen (the “estrobolome”), which directly affects vaginal health [7]. Supporting the gut with Digestzymes or microbial balance protocols is essential.
- Thyroid Function: Low thyroid function slows metabolism and immune defenses, creating a favorable environment for yeast. Optimizing iodine, selenium, and iron intake can help regulate thyroid activity [8].
- If you have not had a comprehensive thyroid panel tested, including autoimmune thyroid markers, click below to get your complete test kit today. Having a full picture of your thyroid could be an essential part of your healing journey. Order your comprehensive thyroid test kit here.
Final Thoughts
Yeast infections after hysterectomy aren’t just “bad luck.” They’re often a signal that the body’s delicate balance between hormones, microbiome, and immune function has shifted. By supporting estrogen balance, rebuilding gut and vaginal bacteria, maintaining liver and thyroid health, and making simple daily choices (like cotton underwear), women can dramatically lower their risk and restore comfort long-term.
References
- Nappi, R. E., & Palacios, S. (2014). Impact of vulvovaginal atrophy on sexual health and quality of life at postmenopause. Climacteric, 17(1), 3–9.
- Cribby, S., Taylor, M., & Reid, G. (2008). Vaginal microbiota and the use of probiotics. Interdisciplinary Perspectives on Infectious Diseases, 2008, 256490.
- Hickey, R. J., & Forney, L. J. (2014). Gardnerella vaginalis does not always cause bacterial vaginosis. Journal of Infectious Diseases, 210(10), 1682–1683.
- Ventolini, G. (2015). Vaginal pH and microbiota during menopause. Hormones, 14(4), 569–576.
- Tait, S. W., & Green, D. R. (2012). Mitochondria and cell death: outer membrane permeabilization and beyond. Nature Reviews Molecular Cell Biology, 11(9), 621–632.
- Schug, T. T., Berry, D. C., Shaw, N. S., Travis, S. N., & Noy, N. (2011). Opposing effects of retinoic acid on cell growth result from alternate activation of two different nuclear receptors. Cell, 129(4), 723–733.
- Kwa, M., Plottel, C. S., Blaser, M. J., & Adams, S. (2016). The intestinal microbiome and estrogen receptor–positive female breast cancer. Journal of the National Cancer Institute, 108(8), djw029.
- Williams, G. R. (2013). Thyroid hormone actions in cartilage and bone. European Thyroid Journal, 2(1), 3–13.