How Sugar Is Affecting Your Liver: The Hidden Root of Fatty Liver Disease
By Dr. Shawn Bladel | July 17, 2025 | Recreated Health
Introduction
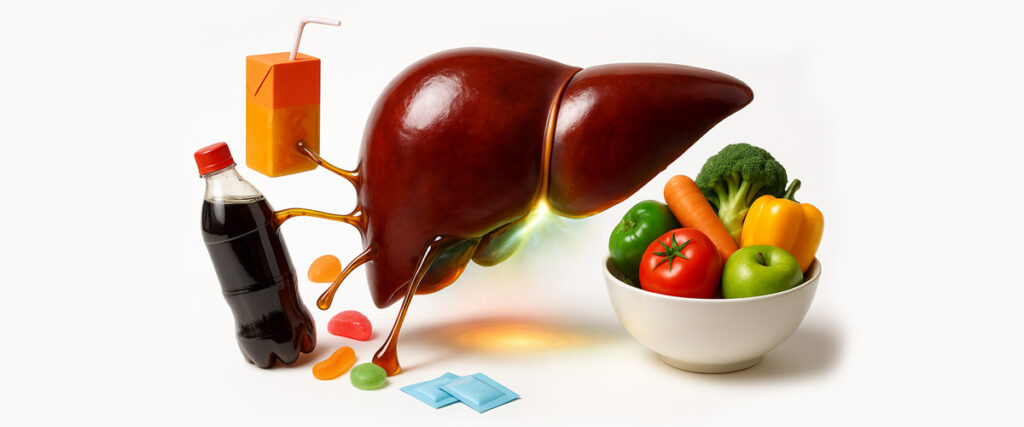
When most people think of liver damage, alcohol is the first culprit that comes to mind. But in reality, sugar—not alcohol—is now the leading driver of fatty liver disease in the U.S. and worldwide.
Millions of people who rarely drink alcohol are being diagnosed with non-alcoholic fatty liver disease (NAFLD). The common thread? A diet heavy in sugar and processed carbohydrates.
At Recreated Health, we often say: Your liver is your body’s filter. If it’s clogged, sluggish, or inflamed, every system in your body suffers.
Your Liver: The Body’s Detox Powerhouse
The liver is one of the hardest working organs you have. Every day it:
- Filters your blood of toxins, chemicals, and pathogens
- Stores and regulates vitamins and minerals
- Processes hormones like estrogen, cortisol, and thyroid hormones
- Metabolizes sugars, fats, and proteins
- Produces bile for digestion
When overloaded—especially by sugar—the liver begins storing fat inside itself. This is the start of fatty liver disease, a condition that affects nearly 1 in 3 adults worldwide [1]. Even children are now being diagnosed due to diets filled with soda, fast food, and refined carbs.
Sugar vs. Alcohol: Why Sugar May Be Worse
Your liver processes sugar in a way very similar to alcohol:
- Both are broken down into fat inside the liver.
- Both create toxic byproducts that increase inflammation.
- Both contribute to scarring and long-term liver damage.
But unlike alcohol—something most people already recognize as harmful—sugar is everywhere and often hidden. Even foods labeled as “healthy” may contain added sugars that silently damage your liver over time.
Fructose: The Real Problem Sugar
Not all sugar acts the same way in the body. The most damaging type is fructose.
- Glucose → can be used by nearly every cell in your body for energy.
- Fructose → can only be metabolized by your liver.
This means when you consume high-fructose corn syrup (HFCS)—common in sodas, condiments, breads, pastas, cereals, and salad dressings—your liver takes the full hit. Over time, this leads to:
- Fat buildup in liver tissue
- Insulin resistance (fueling diabetes, PCOS, weight gain)
- Chronic liver inflammation
As I often tell patients: High-fructose corn syrup is jet fuel for fatty liver.
Processed Grains: Hidden Sugars in Everyday Foods
It’s not just sodas and desserts. Processed grains—breads, pastas, crackers, cereals—break down rapidly into glucose. This spikes blood sugar and insulin.
When insulin levels rise repeatedly, the liver stores more fat internally. Many patients who say, “I don’t eat much sugar,” are unknowingly stressing their liver daily with high-carb, processed foods.
Signs and Symptoms of Fatty Liver
Fatty liver disease often develops silently. Early signs are vague and easy to miss:
- Fatigue or low energy
- Brain fog
- Stubborn belly fat or weight gain
- Hormonal imbalances (PMS, PCOS, low thyroid function)
- Bloating or poor digestion
- Sensitivity to alcohol or medications
As the condition advances, warning signs may include:
- Discomfort or pain under the right rib cage
- Elevated liver enzymes on blood tests
- Signs of prediabetes or metabolic syndrome
How Sugar-Driven Liver Stress Affects Hormones
A sluggish liver can’t process hormones effectively, which leads to:
- Estrogen dominance → worsens PMS, heavy cycles, perimenopausal symptoms
- Insulin resistance → drives PCOS, infertility, and weight gain
- Thyroid dysfunction → poor conversion of T4 to T3, leaving you hypothyroid even with “normal” labs
This is why many women in particular feel the weight of sugar’s damage as mood swings, cycle problems, and stubborn belly fat.
The Emotional Rollercoaster: Sugar, Gut, and Brain
Sugar impacts the gut microbiome as much as it does the liver. When the gut is inflamed and out of balance:
- Neurotransmitter production (serotonin, dopamine, GABA) drops
- The gut lining weakens, causing “leaky gut”
- Anxiety, depression, and irritability become more common
In short, sugar doesn’t just damage your body—it hijacks your mood.
Why Sugar’s Damage Goes Further Than You Think
Sugar-related liver stress has been tied to:
- Skin conditions like acne, eczema, and rashes
- Hormonal imbalances (thyroid, estrogen, insulin)
- Inflammation behind joint pain, migraines, and fatigue
- Weakened immune defenses
Can You Reverse Sugar-Driven Fatty Liver?
The good news: the liver is highly resilient. With the right support, fatty liver disease can be halted and even reversed.
Dr. Shawn’s 3-Step Recreated Approach:
1. Reduce the Sugar Load
- Eliminate sodas, juices, candies, desserts with added sugars.
- Cut processed grains. Swap for fiber-rich vegetables and clean proteins.
- Watch labels—high-fructose corn syrup hides in ketchup, breads, and sauces.
2. Support Liver Detoxification
Your liver is a detox powerhouse—but when it’s overwhelmed by sugar, it gets “stuck.” Fat builds up, bile flow slows, and toxins linger. This is why supplementation and detoxification are so critical for recovery.
Supplements help by:
- Restoring bile flow so fats and toxins can exit.
- Supporting detox pathways (liver, kidneys, gut, lymph) to open the body’s “exits.”
- Replenishing nutrients stolen by sugar and parasites.
- Powering mitochondrial energy so liver cells regenerate.
At Recreated Health, we start with a foundational protocol:
- KL Support → liver and kidney drainage.
- Biotoxin Binder → traps toxic byproducts from sugar metabolism and gut imbalance.
- Bowel Mover → ensures daily elimination, preventing toxin reabsorption.
- BC ATP → restores mitochondrial energy so the liver can repair.
- Digestive Enzymes → ease digestive stress and improve nutrient absorption.
Additional Nutrients for Fatty Liver Recovery
These nutrients provide added healing support:
- N-Acetyl Cysteine (NAC) → boosts glutathione, reduces oxidative stress [2].
- Glutathione → master antioxidant for cellular detox.
- Milk Thistle (Silymarin) → protects liver cells, improves enzyme levels [3].
- Omega-3 Fatty Acids → reduce inflammation and improve insulin sensitivity [4].
- Choline & Inositol → vital for fat metabolism; prevent liver fat buildup.
- Vitamin E → clinically shown to reduce liver fat and inflammation in NAFLD [5].
- Vitamin D3 K2 → deficiency worsens fatty liver outcomes.
3. Rebuild the Gut Microbiome
- Use probiotics and prebiotic-rich foods
- Support gut lining repair with Digestive Enzymes, collagen, and L-glutamine
- Avoid antibiotics, alcohol, and excess sugar
At-Home Testing for Liver & Metabolic Health
To know where your liver stands, at-home testing can provide powerful insight:
- OAT (Organic Acids Test) → shows liver detox stress, gut imbalance, mitochondrial function
- Fingerprick food sensitivity test → helps identify dietary stressors adding to inflammation
- Standard bloodwork (liver enzymes, fasting glucose, insulin) → may show advanced changes
👉 [Order at-home testing kits through Recreated Health here]
Final Thoughts: Protecting Your Liver for Lifelong Health
Sugar isn’t just an innocent indulgence—it’s a hidden driver of liver damage, hormonal chaos, and chronic fatigue.
The empowering truth? Your liver can heal. By cutting hidden sugars, supporting detox pathways, and rebuilding your gut, you can reverse fatty liver and reclaim your energy.
At Recreated Health, we’re here to help you uncover root causes, not mask symptoms.
✅ Next Steps
- 📘 Download the Mitochondrial Blueprint for energy repair strategies.
- 📘 Get the Parasite Detox Blueprint if gut stress and toxins are part of your picture.
- 🛒 Explore foundational supplements in the Recreated Health Store.
- 👨⚕️ Schedule a Consultation for a personalized liver-healing plan.
Your liver is your lifeline. Protect it—and your whole body will thank you.
References
- Younossi Z, et al. Global epidemiology of NAFLD. Metabolism. 2016.
- Lim JS, et al. Role of NAC in reducing oxidative stress in NAFLD. Clin Ther. 2014.
- Loguercio C, et al. Silymarin in liver disease. World J Gastroenterol. 2012.
- Parker HM, et al. Omega-3 fatty acids and liver fat. J Hepatol. 2019.
- Sanyal AJ, et al. Vitamin E for treatment of NAFLD. NEJM. 2010.